Symptoms of Trauma
By Susanna Sweeney, MSC, MBACP, CHT
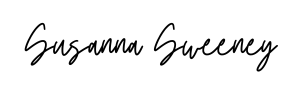
The symptoms of trauma can be far reaching, affecting both your physical and mental health.
- Trauma symptoms can range from mental health conditions such as depression, anxiety and low self esteem to physical symptoms such as chronic pain, migraines, chronic illness and auto-immune conditions.
- Even though these symptoms have been known in the medical and psychotherapeutic communities for decades, what remains poorly understood is how these symptoms relate to the traumatic events that underlie them.
- This has led to a situation where often the trauma link is not made, this is often the case with chronic pain, for example. If there is no physical or medical cause for this pain, there is a good chance the pain could be trauma related- and you won't necessarily know what the trauma was that caused this.
To get the complete up-to-date picture, I asked Dr. Ron Ruden who has devoted long years of his life to the detailed study of the neuroscience of trauma, to talk to me about his take on the issue of trauma symptoms.
Dr. Ronald Ruden on the Symptoms of Trauma
Susanna Sweeney: Could
you give our audience an insight into the symptoms of trauma?
Dr. Ronald Ruden: The first point to make here is that symptom generation is different from traumatization. The landscape of the brain is different for symptom generation than it is for traumatization. So sometimes we will see people who have an experience which is encoded as a trauma, but not until this is altered a little bit more do we get expression in symptomatology.
This gets very confusing from a practitioner's point of view. It can happen all of a sudden- they have a bad day at work and suddenly they start generating symptoms. But these symptoms that are coming from the original traumatization, are only now being triggered because their neural landscape has suddenly become permissive- because the landscape has changed.
This permissiveness gets very confusing because we can’t always make the connections between the traumatic event and the current things that are going on now.
And so we have to take very detailed histories to see if we can pin down the traumatic event. And once we find that, we can then begin to think about removing it.
But the key point here is that a traumatization- the permanent encoding of traumatic memory with that AMPA receptor- does not necessarily produce symptoms straightaway. And the generation of symptomatology requires a permissive landscape, which is a consequence of other types of stressors which changed the landscape.
More About Trauma
Find out Dr. Ruden's comprehensive, novel definition of what trauma is, based on many years of studying the neuroscience of trauma.
Find out exactly what happens in the human brain at the moment of traumatization.
A new science of traumatic encoding of traumatic memories that finally gives answers as to how we can undo the often devastating effects of trauma.
Find out About Havening Techniques®️
Together with his brother Dr. Steven Ruden, Dr. Ronald Ruden founded Havening Techniques®️ using the knowledge he gained from studying neurochemistry.
Having identified how trauma is encoded in the brain they went about finding ways to decode it, with the end result being Havening Techniques®️, a powerful modality for healing the impact of trauma which can be life changing. Learn more here:
- What is Havening and how could it Change your Life? An introduction to the method and what it can do...
- Havening- Interviews with the Founding Fathers: Interviews with Doctors Ronald and Steven Ruden on the origins of Havening Techniques and its development
- Self Havening: How you can use Havening Techniques at home for self help.
Symptoms of Trauma continued
Susanna Sweeney: So, what you're talking about here is the delay between actual events and trauma manifesting in symptoms.
Dr. Ronald Ruden: That's correct. And the symptoms are related to the release of stress hormones and these stress hormones then find places in the brain which are what I would call ‘vulnerable to issues’.
These stress hormones- they can cause issues like increased risk for substance abuse, increased risk for depression, increased risk for obsessive compulsive disorders.
And so it gets really confusing if you- let's say you had a car accident, were traumatized and you walk away and are okay. And then a couple of years later, you have a fender bender which is very minor. The previous dramatic event from the first car accident now is allowed to express its symptoms.
And we see whiplash injuries, which occurred at a moment when there was very little action on the neck. And so we say, how could this be? And then we look at people and say, they are malingering- how could such a small little five mile an hour event have caused the problem? And the answer is, because it's built on a more serious previous event.
Susanna Sweeney: So what we have is accumulated stress factors that accumulate over time and they all interact.
Dr. Ronald Ruden: That's exactly right. And that's why if you do things to down regulate the stress levels, like mindfulness and yoga, we can decrease symptomatology. It works both ways. You can increase the stress by having in place certain circumstances or you can decrease the stress by doing things that down-regulate the stress levels.
Susanna Sweeney: Tell our audience about the breadth of the picture of symptoms of trauma that you see in clinical practice.
Dr. Ronald Ruden: Well, it is astonishing the amount of trauma in the world. Practitioners who are worried that they're going to run out of people to treat because of trauma have nothing to worry about.
I see everything from low self esteem to inability to take a test to the inability to stand in front of a group and talk to inability to maintain relationships for fear of abandonment. These are everyday things and we tend to think of them not necessarily as being pathological, but this is how trauma impacts the individual.
New to Hypnosis?
These articles are designed to help:
Mental Health Symptoms of Trauma
Susanna Sweeney: So tell our audience, what is your opinion about how trauma symptoms are currently being treated in the mental health field in particular?
Dr. Ronald Ruden: Well, one of the things that troubles me is that people go to traditional psychotherapists to treat trauma. And this cannot be touched by talk therapy. Trauma is encoded in the sub-cortical part of the brain.
Now, that doesn't mean that they can't improve symptomatology if they address certain types of other issues in their lives which cause distress and by doing so the symptomatology may improve. But they are not dealing directly with the traumatic base. They are not curing them.
They are treating the landscape of the brain so that the symptomatology does not occur. But if you have a moment where the stressors get worse, then the symptomatology will return. So they go back and forth and back, but never really touch the underlying fundamental problem of this encoded AMPA receptor.
Susanna Sweeney: I have been a practicing psychotherapist for many years. And all of my clients were trauma clients and they often walk in with a diagnosis, maybe from the GP, maybe from the psychiatrist. You have all these different mental health diagnoses that people come with- depression, anxiety and so on. From your perspective do you think that that's helpful?
Dr. Ronald Ruden: I think diagnoses are focusing on just the manifestations of the illness, their symptoms. We tend to treat the individual based on symptomatology. Nothing could be more useless than treating symptomatology.
If you're feeling badly about something, you could not talk yourself out of feeling badly. It's like flypaper you know- you touch it, then you try to get it off to the side and you can't get it off. And until you do remove the original traumatic encoding, you will always be at risk of having symptoms come back in opportune times.
The bottom line is that we can't treat symptoms. We have to treat the underlying subcortical emotional states that pre-chronic, inescapable stress. It releases stress hormones and then symptoms arise from those- when those hormones act on a vulnerable part of your brain.
It's my view that trauma plays a role in almost every single mental health or emotional health condition.
Susanna Sweeney: So when we look at phobias, anxiety, when we look at depression or low self esteem, or low confidence- it doesn't really matter in the end what the symptom is. The clue to resolving them is in the underlying cause, that event or series of events that are encoded traumatically. Right? It doesn't matter what you become symptomatic with- it always goes back to accumulated stress factors. Correct?
Dr. Ronald Ruden: This is similar to what we see in addictive behaviors. People think that alcohol is the cause of alcoholism. Well, if alcohol caused alcoholism, then everyone who had a glass of wine would become addicted to alcohol. That's not the case.
Most people enjoy a glass of wine and they can put it down. And so the landscape of the brain becomes the key for addictive behavior.
I remember back in the early 1990ies, we had a combination of two medications- they raised both dopamine and serotonin. And when we gave that to clients, their cravings for alcohol just went away. They could leave a glass of wine on the table without having to drink it.
And when you looked at that, you said, well, if they were at one time experiencing addiction to alcohol, why by giving these drugs, does it go away? And the answer is that it's not the alcohol, it's the landscape or the brain, which we changed so it would make it non-permissive for a craving response disorder to occur.
And the same thing is true about mental illness or mental symptomatology, you have to get the underlying landscape changed so that we can then allow for the body to heal and not have those symptoms.
Susanna Sweeney: So again, just to be clear, by landscape what we're referring to is the person's neural landscape which is shaped, among other things, by previous incidents of traumatization throughout the person’s lifetime, right?
Dr. Ronald Ruden: Correct, trauma landscapes the brain and you know, we've all experienced getting a bad night's sleep, for example, or if you had a fight with your spouse- that your responses to other people are going to be somewhat different because the landscape of your brain has been changed by stress hormones. And so you want to be able to make an even-keel landscape where when stressors come, you can handle them.
I hope this article and interview on the symptoms of trauma has helped you understand the topic better. In the comments underneath, let our community know what you have learned.
Regards,
Recent Articles
-
Havening Technique Training auf Deutsch
Feb 08, 24 11:02 AM
Havening Technique Training auf Deutsch- Details und Buchung -
Client Testimonials
Oct 06, 23 06:08 AM
Client Testimonials of my Online REPAIRenting® Program that uses various psychosensory approaches for safe and quick transformation -
Smoke Free Thanks to This Amazing Resource
Aug 02, 23 09:26 AM
Oh thank you for this simple resolution to all my worries! I feel like I have had a weight lifted off my shoulders. It is like cheating on giving up smoking.


New! Comments
What do you think? Leave a comment in the box below.